Provides comprehensive descriptions of the 2020 clinical quality measures cqm for the merit based incentive payment system mips quality performance category.
Mips quality measures specifications.
Cms confirmed that the app core quality measure set replaces the current shared savings program quality measure set 2021 proposed rule p.
Please check 2019 clinical quality measure cqm specifications to see changes to existing measures made since the release of the 2018 mips measure specifications.
Measure data may be submitted by individual mips eligible clinicians groups or third party intermediaries.
You must collect measure data for the 12 month performance period january 1 december 31 2020.
This document outlines the documentation requirements for each of the 2019 cms web interface quality measures.
All 2019 cms mips registry and ehr quality measures can be reported with mdinteractive.
There are 6 collection types for quality measures.
The individual measure specifications are detailed descriptions of the quality measures and are intended to be utilized by individual mips.
It is intended to be used as a supplemental resource in conjunction with the 2019 web interface measure specifications posted in the online.
This document contains general guidance for the 2020 quality payment program qpp individual measure specifications and measure flows for mips clinical quality measures cqms submissions.
Measure benchmarks a benchmark is a point of reference against which measures may be compared or.
Only mips eligible apm participants are subject to mips requirements.
The app core quality measure set is the similarity between the app for apm participants and acos.
Cms web interface measure documentation reference guide for performance year 2019 pdf.
Updated 09 01 2020 2020 facility based quick start guide.
The quality data codes listed do not.
Merit based incentive payment system mips quality measure data.
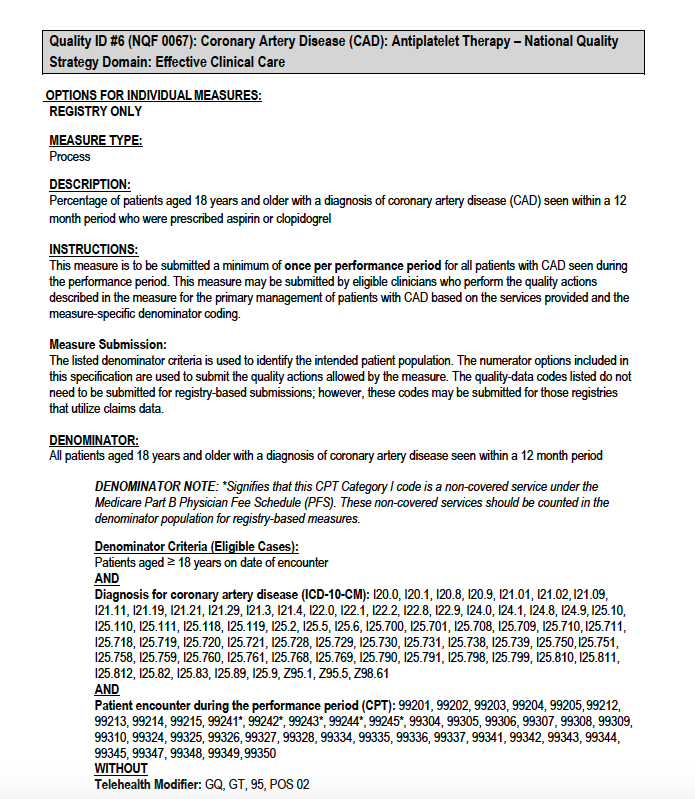
The numerator options included in this specification are used to submit the quality actions as allowed by the measure.
The listed denominator criteria are used to identify the intended patient population.
Please check 2019 mips quality benchmarks to determine how many points each measure can earn for a given performance.